Key Takeaways:
- Intraocular pressure (IOP) is a critical factor in eye health and the development of glaucoma.
- Elevated IOP is strongly linked to optic nerve damage, which can result in irreversible vision loss.
- Early detection and modern management, including innovations in home monitoring, can greatly reduce the risk of glaucoma-related blindness.
Table of Contents:
- Understanding Intraocular Pressure (IOP)
- How Elevated IOP Contributes to Glaucoma
- Mechanisms Linking IOP and Optic Nerve Damage
- Risk Factors for Elevated IOP
- Detecting Elevated IOP
- Managing and Treating Elevated IOP
- Innovations in Monitoring IOP
- Conclusion
Understanding Intraocular Pressure (IOP)
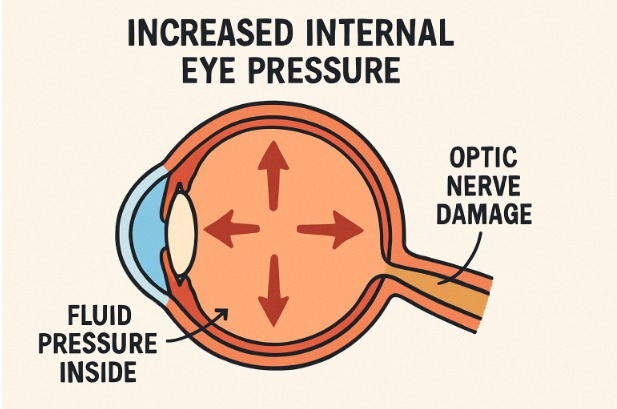
Intraocular pressure (IOP) measures fluid pressure inside the eye. This pressure is regulated by the balance between the production and drainage of aqueous humor, the clear fluid inside the front portion of the eye. Maintaining a healthy IOP level is fundamental for preserving eye structure and function, as deviations either way can impact vision and eye health. Innovations in vision correction, such as the EVO ICL lens, focus significantly on optimal eye pressure and ocular integrity, making advancements in preventing and treating conditions like glaucoma even more important.
Both acute and chronic changes in IOP can disrupt the delicate equilibrium necessary for optimal vision. Chronic elevation, in particular, puts pressure on essential eye structures and is closely tracked in patients at risk for glaucoma, reflecting the eye’s overall health and susceptibility to future damage.
How Elevated IOP Contributes to Glaucoma
Glaucoma is widely recognized as one of the leading causes of irreversible vision loss worldwide. The primary risk factor is heightened IOP, which can stealthily damage the optic nerve over time. Even mild, sustained increases in eye pressure may cause subtle distortion of the blood vessels and impair oxygen delivery to sensitive optic nerve tissues, accelerating the progression of glaucoma. Recent findings show that the relationship between IOP and vision health is not always straightforward; even mildly elevated pressure should be taken seriously in clinical practice.
Optic nerve damage that develops from increased IOP can occur painlessly and without obvious symptoms until significant vision loss has occurred. This highlights the importance of prevention, timely diagnosis, and early intervention, making regular eye exams vital to lifelong ocular health.
Mechanisms Linking IOP and Optic Nerve Damage
The key structure linking elevated IOP to glaucomatous damage is the lamina cribrosa—a sieve-like tissue at the optic nerve head. Persistent pressure can deform this structure, reduce blood flow, and impede the oxygen supply critical for retinal ganglion cells. Prolonged hypoxia inflicts cumulative injury that is not reversible. Damage to the ganglion cells means loss of vision that cannot be restored by simply lowering the IOP later.
Risk Factors for Elevated IOP
- Age: Individuals over age 60 have a higher susceptibility to elevated intraocular pressure and glaucoma.
- Ethnicity: African Americans, Hispanics, and Asians are at a greater risk and tend to develop glaucoma at younger ages compared to other groups.
- Family History: Genetics play a strong role, as those with a family history of glaucoma face increased risks.
- Medical Conditions: Chronic diseases such as diabetes and hypertension are often linked with higher IOP and require careful monitoring.
Detecting Elevated IOP
Routine comprehensive eye exams are essential for early identification of elevated intraocular pressure. Key tests include:
- Tonometry: Measures IOP quickly and painlessly, providing a value that can inform diagnosis and management.
- Ophthalmoscopy: Assesses the optic nerve for subtle changes that could indicate disease progression or acute risk.
Regular screenings are especially important for those with known risk factors, as glaucoma can be asymptomatic in its early stages.
Managing and Treating Elevated IOP
Lowering eye pressure remains the cornerstone of glaucoma therapy. Management strategies are tailored to the individual and may include:
- Medications: Prescription eye drops help to reduce IOP by either reducing fluid production or enhancing outflow.
- Laser Therapy: Modern, minimally invasive procedures like trabeculoplasty improve drainage and can delay or prevent the need for surgery.
- Surgical Interventions: When medications and laser procedures are insufficient, surgical techniques such as trabeculectomy or minimally invasive glaucoma surgery create new drainage pathways for excess fluid.
Early adherence to these treatments is critical, as prompt IOP control can delay or prevent the onset of permanent vision loss.
Innovations in Monitoring IOP
Advances in at-home eye pressure measurement now empower patients to play a more active role in their treatment plans. Devices such as the iCare HOME2 allow for frequent, user-friendly IOP measurement from the comfort of home. This leads to richer, more actionable data for physicians, resulting in truly personalized glaucoma care that adapts to each patient’s daily needs and fluctuations.
Conclusion
Understanding, detecting, and managing intraocular pressure is key to preventing glaucoma and its devastating effects on vision. Regular eye examinations, awareness of personal risk factors, and engaging with the latest therapeutic and monitoring technology can transform outcomes and ensure long-term eye health. Prioritizing timely treatment and embracing advancements such as personalized medicine and at-home IOP monitoring are essential steps in safeguarding your sight for years to come.